The symptoms and treatment of conjunctivitis in dogs are similar to the same ophthalmic disease in humans. Its main danger is a gradual deterioration of vision, fraught with complete loss of visual function.
It is possible to protect your pet from this complication only through careful prevention and timely diagnosis. To do this, you need to know not only the external signs of pathology, but also its main causes.
What is the conjunctiva and how to determine its inflammation
The conjunctiva is the mucous membrane that covers the outer part of the eyeball and the back surface of the eyelid. This thin and transparent shell is necessary for:
- protection from pathogenic microorganisms and foreign bodies;
- wetting the eyes with tear fluid to prevent them from drying out;
- ensuring mobility of the eyeballs and eyelids.
With any disorders, including inflammatory processes, this important organ loses its functionality. The presence of pathology can be understood by changes in the appearance of the mucous membrane. Instead of pale pink, its shade changes to bright red, the smooth surface may become ulcerated, and the previously moderate humidity becomes higher than normal.
The importance of the organ of vision for the animal organism is enormous, since it is in continuous connection with the surrounding external environment, representing an inextricable unity with it. [1]
Diseases that lead to visual impairment make the animal defenseless and unsuited to the struggle for existence. [2]
Such diseases are accompanied by exhaustion of animals and a decrease in productivity. Animals with pathologies of the eyes and their appendage organs become economically unprofitable for owners and farms, because they require special care and can cause some extreme, even tragic situations. [3]
Inflammatory diseases of the conjunctiva and cornea occupy first place in the frequency of visits to a veterinary ophthalmologist, which accounts for more than half of all eye pathologies. [3]
In the conjunctival sac, under completely normal conditions, various microorganisms, including pyogenic ones, are in a latent state, since the eye is an open system communicating with the external environment. At the slightest violation of the “status quo,” the aggressiveness of microorganisms increases, and they can become direct causative agents of the inflammatory process. [3,4]
Follicular conjunctivitis is a chronic inflammation of the conjunctiva, which affects the lymphatic follicles on the inner surface of the third eyelid, less often on the outside and the lower fornix of the conjunctiva. [5,6]
This is the most common form of conjunctivitis in young dogs and less commonly in cats.[1,5,6]
The complexity of the pathogenesis of follicular conjunctivitis, based on inflammation of the lymphatic follicles, which leads to their hyperplasia, as well as the high possibility of the process transitioning to a third eyelid adenoma, also determine the complexity of the treatment of this disease.[2,7]
The long course of the disease leads to pathological changes in the tissues of the conjunctiva, the addition of toxic-allergic and autoimmune components, which aggravates the course of the process and significantly complicates and delays treatment. [7]
Currently, many drugs and methods of treating follicular conjunctivitis have been proposed, which involves surgical intervention and/or the use of new treatment regimens.
We were tasked with developing a scheme for the conservative treatment of follicular conjunctivitis in dogs, as well as comparing the effectiveness of surgical and conservative methods of treating follicular conjunctivitis.
Material and research methods. The objects for the study were sick dogs of various breeds, ages with pathology of the organ of vision and adjacent tissues, admitted to the clinic of the Department of Surgery and Obstetrics of the Law Firm "KATU" NAU, as well as the clinic of Simferopol.
All sick animals were subjected to a general clinical examination with determination of body temperature, pulse rate and respiratory movements. In dogs with clinical signs of damage to the visual analyzer, the eye and surrounding tissues were examined and palpated. Before examination, the conjunctival sac was irrigated with a 0.002% solution of furacillin, which has an antimicrobial effect, the surface of the eye was treated with a 2% solution of lidocaine and, using anatomical tweezers, the inner surface of the third eyelid was turned outward in order to detect inflamed, enlarged lymphatic follicles.
The diagnosis of follicular conjunctivitis was made based on the following clinical signs: swelling of the third eyelid, chemosis, the presence of enlarged lymphatic follicles from the inside of the conjunctiva of the third eyelid (on the side of the eyeball), discharge of mucous or mucopurulent exudate from the inner corner of the eye, soreness of the eyelids, the presence of crusts of dried exudate on their surface, inflammation of the cornea, superficial (conjunctival) or pericorneal injection of blood vessels. In addition to the above symptoms, photophobia, blepharospasm, lacrimation, absence of exudate, and itching were noted.
To conduct the study, we selected 15 dogs of different ages, genders, and breeds with approximately the same clinical signs of follicular conjunctivitis. These animals were divided into two groups. The control group - 8 animals - was treated according to the following scheme:
1. Instillation of a 30% solution of sodium sulfacyl (albucid) was carried out, 3-4 drops 3 times a day. It belongs to the sulfonamide group of drugs; instillations were carried out to prevent the spread of the inflammatory process to other parts of the eye and to treat purulent inflammation of the conjunctiva.
2. We used a 0.1% dexamethasone solution (eye drops) 2 times a day, 2–3 drops. The drug belongs to the group of glucocorticoids and has local anti-inflammatory, antiergic, and antibacterial effects. Locally reduces pain, photophobia, lacrimation, burning sensation.
3. 1% tetracycline ophthalmic ointment was placed in the conjunctival sac; it has a bacteriostatic effect and is effective against G– and G+ bacteria, as well as viruses and fungi.
4. Hydrocortisone 0.5% ophthalmic ointment was also placed in the conjunctival sac. The drug belongs to the group of glucocorticosteroids and has anti-inflammatory, antiallergic, anti-edema and anti-itching effects.
5. Ribotan was used intramuscularly once every 5 days in an amount of 1 ml. The drug has a wide range of biological activity: accelerates regeneration processes, stimulates natural resistance factors, phagocytic activity of macrophages and neutrophils.
The second (experimental) group was also prescribed a 30% solution of sodium sulfacyl, a 0.1% solution of dexamethasone, tetracycline, hydrocortisone ointments and ribotan according to the above scheme, and also scarified the lymphatic follicles with a Volkmann spoon. The goal is to destroy the histohematic barrier of lymphatic follicles that prevent the penetration of drugs.
Scarification was performed as follows: animals were injected with xylazine at a dose of 1–2 mg per 1 kg of live weight (dosage based on the active substance), using Rausch anesthesia to ensure a calm environment during curettage. The conjunctival sac was irrigated with a 0.002% furacillin solution to remove exudate and pathogenic microflora accumulated on the surface of the conjunctiva. Animals were fixed in a lateral recumbent position. A 2% lidocaine solution was instilled onto the surface of the eye, after 3–5 minutes the third eyelid was grabbed with anatomical tweezers, turned outward, and the inner surface of the third eyelid was curetted with a Volkmann spoon. If bleeding occurred, a cotton swab moistened with a solution of adrenaline at a concentration of 1:1000 was applied to the third eyelid.
Animals were observed on days 3, 7, 14, 17, 20 and 25 after the start of treatment.
The effectiveness of treatment was assessed by the change or disappearance of clinical signs.
Results of our own research. For the period 2006–2008 In the clinic of the Department of Surgery and Obstetrics of the Law Firm "KATU" NAU, as well as clinics in Simferopol, 2235 dogs with diseases of non-infectious nature were admitted, of which 257 animals had eye diseases, which amounted to 11.5% of the total number. The most common disease was conjunctivitis in 125 animals – 48.6%. Keratitis took second place - 44 dogs - 17.0%. We recorded 15 animals (5.8%) with follicular conjunctivitis. Based on general clinical studies, it was found that follicular conjunctivitis is more often a consequence of chronic conjunctivitis.
When examining the eye area, the following clinical signs were found: an increase in the size of the third eyelid in 12 (80%) dogs; on its inner surface, the presence of inflamed, enlarged lymphatic follicles was noted in all animals (100%), outflow of mucous exudate from the inner corner of the eye in 8 (53.3%), mucopurulent - in 6 (40%) dogs. Blepharospasm, photophobia, lacrimation, and conjunctival hyperemia were observed in 8 (53.3%) animals.
For the experiment, we were able to select dogs of the same age and breed. Dogs of the first (control) group, numbering 8 animals, whose age ranged from 1 to 5 years, were treated according to the above scheme.
General signs of follicular conjunctivitis in dogs of this group were: an increase in the volume of the third eyelid, on its inner surface the presence of enlarged lymphatic follicles, outflow of mucous or mucopurulent exudate, episcleral and pericorneal injection of blood vessels, corneal opacity in the medial corner of the gray-smoky eye color, hyperemia of the conjunctiva of the eyelids, moderate blepharospasm, mild pain in the eye area, the presence of crusts of dried exudate on the surface of the eyelids.
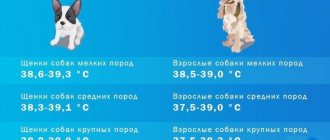
The general condition of the animals was satisfactory, the appetite was preserved, the animals actively ate food, and no signs of general disease were noted. Body temperature was 38.8±0.5°C, pulse – 66.4±3.8 beats/min, respiration – 23.2±3.2 breaths. dv/min
Animals were observed on days 3, 7, 14, 17, 20 and 25 after the start of treatment.
On the 3rd day, a slight increase in the inflammatory reaction was observed, which was manifested by an increase in the number of mucous discharges from the inner corner of the eye, pain, swelling of the third eyelid, and an increase in the size of lymphatic follicles. The general condition is satisfactory, body temperature 38.2±0.4°C, pulse 72.4±4.2 beats/min, respiration 24±0.2 breaths. dv/min
On the 7th day, a decrease in photophobia and lacrimation was observed, and blepharospasm was less pronounced. On the inner surface of the third eyelid, the presence of enlarged lymphatic follicles of pink, rose-red color was observed. Corneal opacity is less pronounced.
On the 10th day, it was noted that pain and swelling of the conjunctiva decreased, and the mucopurulent exudate became more transparent. In 2 dogs with corneal inflammation, corneal opacity decreased. The body temperature of the animals was within 38.4±0.4°C, pulse 60.2±4.3 beats/min, respiration 24±0.4 breaths. dv/min
On the 14th day after the start of treatment, a decrease in hyperemia, pain in the conjunctiva of the third eyelid, and a decrease in its volume were established. Episcleral, pericorneal injection of blood vessels is weakly expressed. General clinical signs were within normal limits.
On the 17th day, it was recorded that one dog had renewed photophobia, blepharospasm, and lacrimation. The absence of such signs was found in 6 dogs, a slight secretion of mucous exudate was noted in 7 animals. Complete conjunctival restoration in one dog.
On the 20th day, the complete disappearance of clinical signs characteristic of follicular conjunctivitis was established in 5 dogs. In one animal, the third eyelid greatly increased in volume, became pink in color, and blepharospasm, photophobia, and copious discharge of mucous exudate were noted. Body temperature was 38.6±0.4°C, pulse 64.5±5.2 beats/min, respiration 22.4±4.2 breaths. dv/min
On the 25th day after the start of treatment, it was noted that complete restoration of the conjunctiva of the third eyelid and the disappearance of lymphatic follicles occurred in 6 dogs (75%). In one animal, blepharospasm, photophobia, abundant mucous exudate from the inner corner of the eye, an increase in the volume of the third eyelid, its hyperemia, pain, and the presence of enlarged pink lymphatic follicles were observed on the inner surface. One dog has a small amount of mucous exudate from the corner of the eye, the third eyelid is slightly enlarged in size, there are yellowish lymphatic follicles on the inner surface, and mild signs of clouding of a smoky color on the cornea.
In the second (experimental) group, which included 7 dogs with follicular conjunctivitis, follicle curettage was additionally used with a Volkmann spoon according to the method described above.
During the initial examination of this group of animals, it was noted that the general condition of 6 dogs was satisfactory, the coat was smooth, shiny, appetite was preserved, and no signs of general disease were detected. The body temperature of the animals in the experimental group was 38.4±0.6°C, pulse 65.6±4.2 beats/min, respiration 18.4±3.6 breaths. dv/min
When examining the eyes of all animals, an increase in the volume of the third eyelid was found, and on its inner surface there were inflamed, enlarged lymphatic follicles of a pink-red color. We noted discharge of mucous and mucopurulent exudate from the inner corner of the eye, episcleral and pericorneal injection of blood vessels in two dogs, and corneal opacification in three. All animals exhibited moderate blepharospasm and photophobia.
On the 3rd day after the start of treatment, it was found that the signs of inflammation intensified, namely: severe blepharospasm, photophobia, copious discharge of exudate mixed with blood, swelling of the eyelids, swelling of the conjunctiva of the third eyelid, its hyperemia, and pain were observed. Episcleral vascular injection became more pronounced compared to the initial examination. Body temperature was within 38.6±0.4°C, pulse 60.5±4.4 beats/min, respiration 22.5±0.4 breaths. dv/min
On day 7, five dogs showed a decrease in signs of inflammation in the eye area. The manifestation of blepharospasm and photophobia decreased. The release of exudate of a mucous nature and mixed with blood was noted in five animals. A decrease in edema, hyperemia, and pain in the conjunctiva of the third eyelid was noted in 4 patients. Body temperature was within 38.4±0.2°C, pulse 60.5±4.2 beats/min, respiration 21.2±0.4 breaths. dv/min
On the 10th day, a decrease in photophobia and blepharospasm was noted in all animals, and a decrease in the secretion of mucous exudate in 5 animals. Reduction of edema, hyperemia, pain of the third eyelid in 6 animals. Absence of episcleral vascular injection in 2 dogs, absence of corneal opacification in one. The general condition is satisfactory, appetite is preserved.
On the 14th day, the absence of photophobia, blepharospasm, and exudate was detected in 4 dogs, and complete restoration of the conjunctiva of the third eyelid was noted. In 2 animals there was no corneal opacification, in one it was mild. A decrease in swelling, pain, and hyperemia of the conjunctiva of the third eyelid was noted in 3 dogs. General clinical signs were within normal limits.
On the 17th day, complete restoration of the conjunctiva of the third eyelid was observed, with no signs of conjunctival inflammation in six animals (85.7%). In one dog, hyperemia of the conjunctiva of the third eyelid and a slight discharge of mucous exudate from the inner corner of the eye were noted. The general condition of all animals was satisfactory. Body temperature 38.2±0.4°C, pulse within 60.2±4.2 beats/min, respiration 20.6±0.4 breaths. dv/min
Thus, we can conclude that the use of curettage of lymphatic follicles on the inner surface of the third eyelid in the complex treatment of follicular conjunctivitis ensured recovery in 85.7% of dogs on the fourteenth to seventeenth days after the start of treatment, while in the control group on the twentieth to twenty fifth day in 75% of animals.
LITERATURE
1. Kopenkin E. P. Eye diseases. – M.: ZooMetVet, 2002. – 274 p.
2. Lebedev A.V., Chervanev V.A. Veterinary ophthalmology. – M.: Kolos. – 2004. – 200 p.
3. Shilkin A.G. Purulent ulcers of the cornea in dogs and cats // Veterinary medicine. – 2004. – No. 5. – P. 53.
4. Cherkay Z.N., Shebits H., Brass V. The use of drops with anandine for conjunctivitis in cats // Veterinary Medicine. – 2007. – No. 5. – P.57.
5. Stekolnikov A. A. Feeding and diseases of dogs and cats. Dietary therapy. – St. Petersburg: Publishing house “Lan”. – 2005. – 608 p.
6. Nimand H. G., Suter P. B. Diseases of dogs. – Moscow: Aquarium, 2001. – 540 p.
7. Parshin A. A., Sobolev V. A., Sozinov V. A. Surgical operations in dogs and cats. – M.: Aquarium, 2003. – 232 p.
Maslennikova Yu. B.
Causes of conjunctivitis in dogs
The causes of conjunctivitis in dogs are divided into primary and secondary. In the first case, the pathology acts as an independent disease, and in the second it is a complication. Because of this, very often self-medication only smoothes out existing symptoms, provoking the development of a chronic form.
The inflammatory process in the conjunctival area develops under the influence of the following factors:
- Chemical compounds.
Close contact with washing powders, construction paint or other chemicals can result not only in irritation, but also in complete loss of visual function.
- Infections of various etiologies.
Refers to secondary causes. They are caused by viruses, bacteria and fungi that infect the mucous membrane directly or through neighboring organs.
- Mechanical injuries and pathologies of the visual organs.
A speck stuck in the eye or ingrown eyelashes causes severe discomfort, causing the animal to constantly itch. This leads to damage to the conjunctiva and the penetration of secondary infections.
- Weakened immunity.
Colds and chronic diseases worsen the body's defenses, causing multiple complications.
- Allergies.
Redness, swelling and increased tearing are due to exposure to the allergen.
- Inflammatory processes in neighboring areas.
Existing pathology, left without treatment, can spread to the eye shell.
- Irradiation.
Vision problems are caused by radiation, X-rays and ultraviolet rays.
- Parasitosis.
The vital activity of parasites leads to acute intoxication, affecting the functionality of the eyes and other organs.
The risk group includes breeds with bulging eyes: Chihuahuas, pugs, Pekingese. They can get injured even when sniffing grass, since their mucous membranes are practically unprotected.
Infectious forms of inflammation of the conjunctiva
Conjunctivitis is an inflammation of the conjunctiva that occurs in response to damage. Damaged conjunctiva may react with the development of hyperemia (redness), edema (chemosis), discharge, and the formation of follicles. In dogs, conjunctivitis (inflammation of the conjunctiva) is rarely a primary disease and is almost always a consequence of other eye diseases or systemic diseases. When assessing a dog with an inflamed conjunctiva, a physician should always look for the underlying cause or causes of conjunctivitis and treat those specifically, avoiding nonspecific treatments.
Causes and types of eye infections
Many owners with several dogs, as well as other pets, are interested in whether conjunctivitis in a dog is contagious. Also, sometimes they themselves are afraid of catching eye inflammation. But if canine conjunctivitis is safe for a person, then for another dog it can pose a threat.
Infections that cause inflammation of the conjunctiva:
- Lyme disease/tick-borne borreliosis (Borrelia burgdorferi);
- Distemper of dogs;
- Canine oral papillomavirus;
- Leishmaniasis (Leishmania donovani, Leishmania infantum);
- Trypanosomiasis (Trypanosoma brucei, Trypanosoma vivax);
- Herpes virus infection of newborn puppies;
- Infectious hepatitis virus type 1 (CAV-1);
- Monocytic ehrlichiosis (Ehrlichia canis);
- Rickettsial disease is Rocky Mountain spotted fever (Rickettsia rickettsii).
Bacterial infection may not be the primary cause of conjunctivitis in dogs. Bacterial conjunctivitis develops when a predisposing disorder alters normal bacterial homeostasis, which stimulates bacterial proliferation. These disorders may be eyelid abnormalities (ectropion, entropion, lagophthalmos, trichiasis, etc.), trauma, foreign body, and possibly chronic eyelid skin pathology (blepharitis, pyoderma, seborrhea). Keratoconjunctivitis sicca is another common cause of bacterial growth in the conjunctiva.
A thorough eye examination will rule out most predisposing causes of bacterial conjunctivitis. Cytological smears show neutrophils and bacteria. In chronic and recurrent cases, aerobic bacterial culture and antibiotic sensitivity testing are indicated, but resistant bacteria are rarely the cause of conjunctivitis. In cases of chronic and recurrent conjunctivitis, there is always a predisposing and hidden cause of this disease.
Comparative diagnostics
| Disease | Ophthalmic signs | Specific clinic | Diagnostics |
| Carnivore plague | conjunctivitis, keratoconjunctivitis sicca, optic neuroretinal dystrophy, chorioretinitis, corneal ulceration | Damage to the skin, mucous membranes, internal organs, nervous system disorder | Bioassay, serological diagnostics are used in exceptional cases |
| Chlamydia | conjunctivitis | Damage to the genitourinary system | Serology, allergy tests |
| Mycoplasmosis | conjunctivitis | Damage to the respiratory and digestive organs, arthritis, lameness | Serology, smear microscopy |
| Infectious hepatitis | uveitis, keratitis | Inflammation of the respiratory and digestive organs, central nervous system depression | Long-term precipitation reaction |
| Leptospirosis | conjunctival petechiae, hemorrhages under the conjunctiva | Jaundice, fever, lower back pain | Detection of antibodies in the blood, isolation of bacteria from urine, aborted fetus |
Therapy for contagious conjunctivitis in dogs
Treatment of bacterial conjunctivitis in dogs involves ruling out the underlying cause and using topical broad-spectrum antibiotics. For viral and bacterial conjunctivitis, it is recommended to use ophthalmoferon:
- 1-3 days of treatment – instill into the conjunctival sac 5-6 times a day;
- subsequent days – 3-4 times a day;
- course of treatment until complete recovery.
When an infectious cause is established, specific therapy is used. So, for leptospirosis, streptomycin and serum against leptospirosis are effective. For canine distemper, immunostimulating and antiviral medications are prescribed.
Main symptoms and accompanying signs
The severity of symptoms depends on the form of the disease. The most difficult to notice is the chronic form, characterized by prolonged development and mild symptoms.
The main symptoms of conjunctivitis in dogs can be seen in the photo. The mucous membrane turns red and swells, so the palpebral fissure gradually narrows.
Other signs depend on the type of pathology and may include:
- excessive tearing and itching;
- severe pain when blinking;
- swelling of the throat and eversion of the eyelid;
- formation of red blisters in the third eyelid;
- photophobia;
- the appearance of bald patches in places where pus accumulates;
- serous or purulent discharge with an unpleasant odor, sticking the eyelids together when dry;
- bleeding of the eye and death of its tissues.
When diagnosed in the early stages, the disease can be cured within 2 weeks. Otherwise, recovery may be delayed, since the chronic form tends to recur.
What kind of disease is this
Conjunctivitis is an inflammation of the connective membrane, that is, the conjunctiva. It covers the surface of the eyelids and comes into contact with the outside of the dog's eye. The conjunctiva is responsible for the immunity of the eye - any attack of pathogenic organisms on the organ of vision primarily falls on this membrane. Therefore, it is extremely important to keep the conjunctiva healthy .
Types of pathology
For the reasons that caused inflammation of the conjunctiva, the disease is divided into:
- Primary – develops as an independent, separate symptom. For example, if some foreign object gets into the eye.
- Secondary – if it is a consequence of any other disease (any eye diseases, viral diseases, internal pathologies).
According to the speed of development and duration of inflammation:
- Acute – develops rapidly, symptoms are pronounced (burns, viruses, infections).
- Chronic – periodically recurring symptoms, mild manifestations of pathology (irritants, allergies, lack of vitamins).
According to the nature of discharge from the eyes:
- Catarrhal (discharge transparent, whitish or with a brown tint).
- Purulent (yellow or green discharge).
- Follicular (light discharge, an important distinguishing feature is small seals on the inside of the eyelid and on the third eyelid).
Depending on the involvement of the organ of vision in the inflammatory process, conjunctivitis is divided into:
- unilateral (inflammation in only one eye);
- bilateral (when both eyes are affected).
Risk group
Animals of all sizes and ages are susceptible to conjunctivitis. However, we can highlight some points when a dog has a greater chance of encountering pathology:
- dogs of brachycephalic breeds and breeds with drooping eyelids;
- young and elderly individuals are more susceptible to conjunctivitis of an infectious nature;
- animals prone to allergies (both food and atopic);
- In short dogs, a pathology often occurs - dry keratoconjunctivitis, when there is a violation of the production of tear fluid in sufficient quantities (usually treated surgically).
Routes of infection
The main reasons why conjunctivitis develops in dogs:
- injury to the eyelid or eye;
- entry of a foreign body;
- allergies of any nature;
- bacterial;
- viral;
- contact with toxic substances in the eyes;
- internal non-communicable pathologies;
- improper growth of eyelashes;
- any pathology of the organ of vision.
Types of pathology
Due to the appearance and severity of symptoms, the disease is divided into 7 varieties. They all involve different treatment methods.
Allergic
Allergic conjunctivitis in dogs occurs soon after contact with allergens (dust, pollen, tobacco smoke, household chemicals). It is accompanied by profuse tearing and mild swelling. Despite the rather harmless signs, you should not ignore it. Otherwise, this type may develop into purulent.
Purulent
Purulent conjunctivitis in dogs is accompanied by the discharge of yellow-green or white pus from both eyes. Most often, pathogenic microorganisms are to blame for its appearance, therefore, in addition to redness of the conjunctiva, the patient experiences temperature fluctuations, apathy and loss of appetite.
Catarrhal
Catarrhal conjunctivitis in dogs is characterized by an abundance of mucus in the exudate formed. During sleep, it dries out, so when waking up, the animal opens its eyes with great difficulty.
Follicular
Follicular conjunctivitis in dogs is the most difficult to tolerate, as it causes very severe pain. Appears as a result of irritation or damage to the lymphatic follicles inside the eyelids. Under the influence of negative factors, they become inflamed and change their color to crimson.
Viral or bacterial
The infectious variety is caused by viruses or bacteria. A pet with characteristic symptoms of chlamydia, herpes, adenovirus or distemper should be isolated from other pets as soon as possible to prevent the spread of infection.
Phlegmonous
The phlegmonous or parenchymatous appearance is distinguished by the fact that it penetrates into deeper layers. It affects the parenchyma - the tissue covering the internal organs. Part of the conjunctiva bulges outward and bleeds even from a light touch.
Fibrinous
Accompanied by the appearance of whitish films consisting of fibrin protein. They can flake off or go deep into the mucosa, causing necrosis and heavy bleeding.
Types and symptoms of the disease with photos
First of all, the disease can be divided into 2 types: primary, when the cause of the problem lies on the surface (eye injury, sand ingress, etc.), secondary, when conjunctivitis develops due to infection (distemper, adenovirus, hepatitis).
The general classification divides conjunctivitis in dogs into 4 types. Each of them has its own causes, symptoms, course, treatment and complications.
Follicular conjunctivitis in dogs
A chronic breed disease, often found in dogs with drooping lower eyelids . It is characterized by inflammation of the third eyelid due to enlargement of the gland, the appearance of follicles (small bubbles with liquid). It is treated either with antibiotic ointments and drops, or with surgery.
Symptoms of follicular conjunctivitis:
- Itching, lacrimation, whitish or yellowish purulent discharge;
- Swelling of the eyelid and conjunctiva, redness;
- Dried crusts on the surface of the eyelids and eyelashes;
- Pain, swelling of the eye, closure of the palpebral fissure;
- Photophobia;
- Increased body temperature.
How is diagnostics carried out and why you can’t make a diagnosis yourself
Diagnosis in a veterinary clinic involves an external examination of the affected eyes, taking a sample of blood and exudate. If injury or allergy is suspected, an x-ray or ultrasound may be required. Based on the results obtained, the doctor determines the root cause and type of pathology, as well as the susceptibility of the pathogen to antibiotics.
Self-diagnosis and treatment at home are unacceptable due to the variability of possible negative factors. At best, uncontrolled use of eye drops will simply smooth out the existing symptoms, and at worst, it will aggravate the real problem.
Treatment of purulent conjunctivitis
After rinsing, it is necessary to place antibiotic ointments and medicinal eye films under the lower eyelid. This procedure is performed 3-4 times a day. Very effective is the subconjunctival administration of a mixture that includes an antibiotic (10,000-20,000 units of kanamycin), 1 ml of novocaine solution, 0.1 ml of hydrocortisone. Very often, the doctor suggests performing a cranial cervical sympathetic ganglion block. A course of antibiotics must be administered intramuscularly; the duration depends on the initial condition of the patient. In addition to them, sulfonamide drugs are prescribed.
Treatment of conjunctivitis in dogs at home
The main therapy is conservative. Surgery is used only in advanced situations when there is a high risk of vision loss.
First of all, they fight the underlying disease, and after the condition has stabilized, they eliminate the accompanying symptoms. Depending on the diagnosis, your four-legged pet may be prescribed:
- antivirals and antibiotics used to treat purulent conjunctivitis in dogs caused by viruses or bacteria;
- antihistamines and glucocorticosteroids used for allergies;
- analgesics, antipyretics and anti-inflammatory.
Particular attention is paid to washing and treating affected eyes. For this, drops, ointments and herbal decoctions are used.
Strictly follow the veterinarian's instructions
Remember that only a doctor determines how to treat conjunctivitis in a dog at home. Do not try to replace prescribed drugs with human analogues, increase or decrease the dosage. This may cause severe side effects.
Some types of pathology are dangerous not only for domestic animals, but also for humans. When handling your pet, be sure to use protective gloves and wash your hands after each contact.
Drops, ointments and their dosage
To treat conjunctivitis in dogs, drops and ointments that have antibacterial and anti-inflammatory effects are used. Recommended medications and dosages can be found using the table.
| Name of the drug | Mode of application |
| 2-3 drops 1 time per day for 1-2 weeks |
| 1-2 drops twice a day for 5 days |
| 1-2 drops every 1-4 hours until symptoms disappear |
| 1-2 drops every 5 hours until symptoms disappear |
| 1-2 peas under the lower eyelid up to 5 times a day for 1 week |
| 1-2 peas under the lower eyelid twice a day until symptoms disappear |
| 1 cm of ointment on the cornea after each rinse for 1 week |
Please note that the dosage and frequency of use may be adjusted by your veterinarian. All of these drugs should be used alternately, since with prolonged use of only one active substance, bacteria lose susceptibility to it.
Eye hygiene: rinsing and instillation
Before instilling drops or applying ointment, the eyes are washed with a solution of furatsilin, chamomile decoction or plain warm water. This is necessary to remove dried crusts of pus and dirt adhering to them. All manipulations should be carried out with a lint-free cotton pad so as not to damage the cornea.
After treatment, the drug prescribed by the doctor must be dropped onto the mucous membrane or placed in the corner of the eye, slightly pulling the lower eyelid. The treated eye should be closed for a few seconds and massaged a little so that the product is evenly distributed.
If it comes to surgery
Surgical intervention is resorted to when the disease is chronic, as well as when the follicular form is not amenable to conservative treatment. Most often, the operation is limited to partial excision of the affected tissue. This does not affect the quality of visual function, since after some time the removed areas regenerate.
Only enucleation, that is, cutting off the eyeball, can worsen the quality of life. This operation is resorted to only in the most serious cases, when the life of a four-legged patient is at risk.
Keratoconjunctivitis sicca
Causes:
- Drug-induced: Sulfa drugs such as sulfadiazine (eg, trimethoprine/sulfadiazine) and sulfasalazine may cause the development of SBS.
- autoimmune: In 75% of idiopathic SCC, autoimmune destruction of the lacrimal gland may occur.
- Surgery-related: SCC may clinically develop as a result of removal of a prolapsed third eyelid gland. It often develops several months to years after the gland is removed.
- Orbital and supraorbital trauma can result in direct injury to the lacrimal gland or damage to the nerve supplying the lacrimal glands (ie, damage to the facial nerve can lead to the development of SCS).
- Distemper: Canine distemper virus can infect the lacrimal gland and the third eyelid gland and lead to the development of acute SBS with temporary or permanent dysfunction.
- idiopathic: senile atrophy of the gland can be one of the idiopathic causes.
Clinical signs and diagnosis
Clinical signs may be more common during hot, dry seasons, when tear evaporation is greatest. Often, keratoconjunctivitis recurs periodically after treatment or spontaneous recovery (improvement of living conditions, elimination of the cause).
- Red eye syndrome: redness is caused by conjunctival hyperemia.
- Blepharospasm: Accompanied by enophthalmos, it is often the first sign and occurs due to pain and discomfort.
- Dry, dull cornea ± corneal ulcers.
- Corneal vascularization and pigmentation: In chronic cases, superficial and deep corneal vascularization and pigmentation may occur.
- Dryness of the nostril on the affected side.
- Mucus and mucopurulent discharge: When the aqueous phase of the precorneal tear film (PTF) is missing or the fatty phase is disrupted, mucus accumulates and is not washed away by the lacrimal system.
The mucus is usually a viscous gray substance, but it can become mucopurulent if a secondary bacterial infection occurs. Animals with red eye and mucous or purulent discharge should be examined for the presence of SBS (Schirmer's tear test).
Qualitative abnormalities of the tear film (disturbance of the lipid or mucous phases with a normal aqueous phase) can also cause the appearance of clinical signs of SBS. For diagnosis, the Schirmer tear test is used:
- norm in dogs >15 mm tears/min
- TSS time < 15 mm/min in dogs indicates SBS if accompanied by clinical signs (mucous discharge, conjunctival hyperemia or keratitis).
Treatment methods for keratocojunctivitis sicca
If the cause is the use of drugs, the drug is stopped. The first line of defense is local administration of cyclosporine 2 times a day:
- animals with Schirmer test results <2 mm/min have a 50% chance of responding positively to cyclosporine;
- dogs with results >2 mm/min have an 80% chance of responding to this therapy.
It is important to diagnose autoimmune SBS and begin early treatment before the lacrimal glands atrophy secondary to chronic inflammation. A small amount of normal tissue producing watery tears must be present for cyclosporine to be effective. It may take 8 weeks or more for cyclosporine to relieve inflammation and allow the tear gland to function. Therefore, intensive local therapy with ointments containing antibiotics and the introduction of artificial tears are necessary until tear production returns to normal.
Topical antibiotic therapy is necessary to treat and/or prevent secondary bacterial conjunctivitis. Dogs with KBS often develop corneal ulcers that become easily infected. It is impossible to over-water the eye, so owners should be encouraged to administer medications as often as possible (4-8 times daily). Surgical removal of a prolapsed third eyelid gland may predispose the animal to the development of SBS. Cyclosporine therapy must be continued lifelong or clinical relapses will occur (as well as increased destruction of the lacrimal gland). Initially, cyclosporine is administered 2-3 times a day. After tear production returns to normal, the frequency of drug administration can be reduced to 1-2 times a day.
Artificial tears help replace the precorneal tear film Preservative-free artificial tears cause less eye irritation. Products based on methylcellulose are more viscous and have a longer lasting effect.
Lanolin-based ointments are often used. Salivary gland transplant - This treatment method is used in dogs when treatment with cyclosporine is ineffective and when the owner is unable to administer the drugs frequently enough.
Possible complications and consequences
An advanced disease is fraught with transition to a chronic form and loss of vision. With allergic conjunctivitis, a dog may develop a complication in the form of bronchial asthma, with fibrinous conjunctivitis - curvature and scarring of the eyelids, and with purulent conjunctivitis - sepsis. Distemper and other dangerous infections threaten death, since after the incubation period the patient’s condition sharply worsens.
Diagnosis of the disease
Conjunctivitis is usually accompanied by discharge from the eye. If the discharge is abundant and clear, then this is severe conjunctivitis, which can be caused by foreign bodies, improperly growing eyelashes, physical irritants (such as wind) and various allergens. Allergic conjunctivitis is accompanied by itching, the dog rubs its eyes.
Detected changes:
- the presence and nature of the exudate (serous, fibrinous, purulent, hemorrhagic, mixed);
- mucous threads;
- fibrin threads;
- bacteria;
- mycelium;
- heartworms;
- demodex (in a smear, on the eyelashes);
- cellular debris;
- pseudomembrane;
- the presence of inflammatory cells (neutrophils, eosinophils, basophils, lymphocytes, plasma cells, histiocytes);
- the presence of giant and syncytial multinucleated cells;
- the presence of dystrophic or necrotic epithelial cells (vacuolation of the nucleus, vacuolation of the cytoplasm, karyopyknosis, karyorrhexis, karyolysis, nuclear fragmentation);
- keratinization phenomena;
- the presence of pathological inclusions in the nucleus or cytoplasm (cocci, initial or elementary bodies, viral bodies);
- changes in nuclear-cytoplasmic ratio;
- hyperactive goblet cells.
Discharge from one eye suggests local inflammation or a foreign body. If both eyes are sick, then the dog has a common infection.
Pus-like discharge, thick, viscous, often in the form of crusts on the eyelids, indicates a bacterial cause of the disease (purulent conjunctivitis). It is necessary to culture bacteria and select the most effective antibiotics for highly qualified treatment. If the disease continues for a long time, it becomes chronic. Deep-rooted infection is difficult to detect. In such cases, the lacrimal system is affected and the eye becomes dry (keratoconjunctivitis sicca).