Causes of third eyelid prolapse
Reasons that can cause prolapse of the third eyelid:
- Reduction or loss of innervation of the muscles surrounding the eyeball (a number of neurological diseases can lead to this).
- Relaxation of the muscles around the eyeball, for example, from the use of tranquilizers, due to poor (critical) physical condition, etc.
- Weakening of the third eyelid ligaments.
- Tumors, cysts or inflammatory diseases of the third eyelid.
- Any source of pain in the eyeball area. Pain stimulates the eye to move deeper into the orbit.
Diseases that cause pain and prolapse of the third eyelid:
— Entropy is abnormal eyelash growth that causes irritation of the cornea.
— Corneal ulceration, foreign body, laceration.
- Injuries to the eyelids.
— Dry conjunctivitis, or dry eye syndrome.
— Acute glaucoma (sudden increase in pressure in the eye).
- Dislocation of the lens.
Neurological causes of third eyelid prolapse:
Horner's syndrome (Horner) is a neurological disease that occurs due to dysfunction of the sympathetic nervous system. The sympathetic nervous system controls many glands and involuntary functions in the body. Third eyelid prolapse is one of four clinical signs (ptosis, miosis, enophthalmos) that develop in association with Horner's syndrome. Horner's syndrome usually affects only one eye.
Damage to the cranial nerves that control the muscles around and behind the eyes can lead to third eyelid prolapse
Tetanus is a bacterial infection that produces a neurotoxin. These bacteria usually enter the body through a wound. Tetanus toxin causes convulsions and paralysis, as well as bilateral prolapse of the third eyelids. Fortunately, tetanus is rare in dogs.
Why does a dog have a third eyelid?
The semilunar fold in dogs acts as an additional protection for the organ of vision.
When there is a risk of collision with objects, the semilunar fold closes the eyeball first. This kind of nictitating membrane works instantly, protecting the dog’s eye from foreign objects entering it, as well as in case of danger, for example during an attack by other animals.
Also, when blinking, it removes small foreign bodies - dust particles - from the surface of the eyeball.
Lymphoid tissue, which is part of the third eyelid, performs a protective function against infections.
The lacrimal gland, located at the base of the third eyelid, produces tear fluid necessary to moisturize the outer membrane of the visual apparatus.
Structure of a dog's eye
Home care
Vision remains normal unless the third eyelid covers more than 1/2 of the eye. Keep your pet in a safe place until the cause of the problem is determined.
You should not give dogs "redness relief" eye drops intended for humans, as this will not solve the underlying problem and may cause irritation.
(c) Veterinary center for the treatment and rehabilitation of animals “Zoostatus”. Varshavskoe highway, 125 building 1. tel.
Pathology is a manifestation of many diseases and is not an independent disease. In some breeds of dogs, the third eyelid protrudes slightly forward, which is not a pathology and does not require treatment. Ipasmoma is an immune-induced thickening and widening of the outer edge of the third eyelid, found in German shepherds in combination with chronic superficial keratitis. Prolapse of the third eyelid can occur with an overdose of tranquilizers (vetranquil).
With an acute onset and unilateral damage, the most likely symptoms are: pain in the eyeball (corneal ulcer, uveitis, etc.) and an inflammatory process in the orbit (abscess, cellulitis). In middle-aged and older animals with unilateral lesions and no pain, the cause is often a neoplasm of the orbit or third eyelid. It is necessary to pay attention to other possible symptoms of eye pathologies, which may become the etiology of third eyelid prolapse. A disease of the nervous system, more precisely, damage to the sympathetic trunks, also leads to prolapse of the third eyelid. In this case, the causes of pathologies of the nervous system can be different, including infections and poisoning, intoxication in other diseases of the internal organs. Bilateral prolapse of the third eyelid is also possible with systemic diseases (dehydration, cachexia) and with constitutional features (more often in young animals). In cases where the gland of the third eyelid falls out, swelling of the medial part of the third eyelid occurs, the rest of its parts are usually not changed.
Testing of the autonomic nervous system can confirm an inherited autonomic disorder. With concomitant Horner's syndrome, a chest x-ray is indicated (it is possible to detect the causes of sympathetic denervation, identifying metastases in the lungs). If a tumor is suspected, an ultrasound of the orbit is indicated, possibly followed by a CT or MRI. A complete ophthalmological examination is required. With a unilateral process, it can be assumed that the pathology is localized in this eye or its auxiliary organs; the medial part of the third eyelid and the conjunctival fornix must be carefully examined to detect a foreign body or symblepharon. Plasma cells and lymphocytes are detected in impression smears of the third eyelid if a plasmama is suspected. Sometimes, with space-occupying formations, it is necessary to resort to diagnostic surgery and a biopsy of the affected tissue.
Treatment of third eyelid prolapse
In cases where the loss is associated with another pathology, it is necessary to treat it. If the cause of the symptom is pain, then it is necessary to eliminate the factors causing it (remove the foreign body, treat the underlying disease). Orbital abscess and cellulitis usually respond to antibiotic therapy. For neoplasms, exenteration is recommended. Microphthalmia usually does not require treatment, but if pain and recurrent conjunctivitis occur, enucleation of the eyeball is necessary. In Horner's syndrome with an identified cause, the underlying disease is treated, and in case of an unknown cause (50% of cases), the symptoms disappear on their own after 4-12 weeks. In case of intoxication, in addition to the main therapy, detoxification therapy will help. Surgical removal of the entire third eyelid is indicated only for its neoplasms and is not used for secondary eyelid prolapse. If tumor cells are detected at the edges of the surgical incision, cryodestruction or radiation therapy is required.
Pathogenetic treatment of plasmoma can be controlled with local treatment throughout life. Corticosteroids (0.1% dexamethasone or 1% prednisolone acetate) are used initially every 6 hours, and after improvement - every 24 hours.
On the subject: Surgical treatment of third eyelid prolapse
Etiology
The disease is most often recorded in dogs of the French and English bulldogs, pugs, chihuahuas, Chinese Pekingese, bullmastiffs, cocker spaniels, cane corsos, and toy terriers.
The fact that the incidence rate, according to statistical data, is more frequent in the breeds listed above, speaks of genetic inheritance and it is this that determines the structural features of the third eyelid in dogs.
Experimentally, with confirmation by histological studies, it was determined that in these breeds the connective tissue, subcutaneous tissue and the gland itself located under the third eyelid have a looser structure, and the ligament holding the gland is thinner, which contributes to its growth.
A prerequisite for pathology may be a pathogenic microflora, which, with a decrease in immunity, at a certain point acquires increased virulence and causes the gland tissue to react with proliferation.
Since the listed rocks have iron that is somewhat larger in size, it tends to shift and come out of its bed. There is a partial infringement of it by the edging of the third eyelid, and then the eyelid itself turns out, unable to hold the gland. This process sometimes results in deformation of the third eyelid cartilage.
The process, as a rule, begins with one eye, but after a while it moves to the second.
Lacrimal gland prolapse: general points and causes
In the practice of a veterinary ophthalmologist, prolapse, or inflammation of the lacrimal gland, is diagnosed in cats and dogs, regardless of age, gender and breed. Although, according to observations, owners often contact:
- Chihuahuas, mastiffs, Newfoundlands, beagles, French bulldogs (dogs);
- Persians, exotics and British (cats).
It is noteworthy that in “nobles” prolapse is rare, as well as in animals that are less susceptible to genetic transformations and also have a normal skull structure. Brachycephals, due to excessive deformation of bones and soft tissues and anatomical changes in the lacrimal glands, including animals with bulging eyes, are susceptible to prolapse.
Important! But in older dogs, examination will require differentiation from a tumor (neoplasm). Since outwardly at first the clinical picture is similar.
Prolapse and cartilage crease
The reasons are not fully understood, but there are a number of factors that provoke prolapse:
- weakness of the ligaments (genetically determined cause or injury in which the ligaments lose their elasticity or rupture);
- eversion of the T-shaped cartilage (prolapse with eversion is diagnosed).
Separately, we can mention neoplasms (adenoma, older animals are more often predisposed) and hyperplasia of the lacrimal gland in leukemia, although these pathologies would be more correctly considered as separate ones with the involvement of the third eyelid in the process.
What a pet owner needs to know
Lacrimal gland cyst
Prolapse of the lacrimal gland of the third eyelid needs to be treated! This is the unequivocal opinion of all specialists, since in addition to a cosmetic problem, there is a risk of injury from paws and claws when the pet tries to remove visual interference. Scratching and violation of tissue integrity create a direct gateway to infection, bacterial contamination, the “bag” becomes even more inflamed and suppurates. Subsequently, the inflammatory process spreads to the external and then to the deep structures of the eye, and the pet may completely lose vision.
With prolapse of the lacrimal gland of the 3rd century, the gland itself is in the wrong position, tissue trophism worsens, its functions partially disappear, and tear production decreases. As a result, there is a risk of developing dry keratoconjunctivitis, the iris is poorly wetted, painful sensations occur, damage to structures and the development of cartilage fractures occur.
Important! It is a mistake to reset the prolapsed lacrimal gland yourself (with your finger, tweezers). It will not be possible to achieve complete fixation, but it can cause injury and infection. Sometimes it corrects itself, and the owner calms down until another prolapse occurs.
You should not confuse the two concepts - adenoma of the lacrimal gland and prolapse and remove the gland without differentiation, which increases the likelihood of impaired tear production and the development of keratoconjunctivitis sicca. It is better to resort to a proven standard solution - reduction and fixation of the ligament, which takes 20-30 minutes using the new ophthalmological equipment of the Ros-Vet VC and under general anesthesia with local anesthesia.
Symptoms of hair loss
The emergence of the third eyelid beyond its normal boundaries, as well as its swelling, is a serious cause for concern. The non-physiological position of the membrane is a signal of certain diseases or injuries. In addition to the fact that the third eyelid becomes visually noticeable, other symptoms are noted. In cases where the causes of the unpleasant phenomenon are directly related to the eyes, redness of the conjunctiva occurs, the release of an increased amount of tear secretion, the appearance of purulent discharge in the corners of the eyes, and involuntary spasm of the orbicularis oculi muscle. A burning sensation in the eyes affects the cat's behavior. She tries to avoid the light and scratches her eyes with her paws.
If the problem is caused by systemic or infectious diseases, then the cat will exhibit symptoms characteristic of such conditions. These include general weakness, decreased activity, loss of appetite, and increased temperature. If the problems are related to the digestive tract, then frequent or episodic vomiting and diarrhea are possible. As the process drags on, the animal loses weight and the condition of its coat deteriorates. In rare cases (with Horner's syndrome), paralysis or paresis of the limbs and facial nerve occurs.
Sometimes third eyelid prolapse is confused with lacrimal gland prolapse because these conditions are visually similar. To distinguish these problem situations and understand the solutions, it’s worth watching this useful video:
Pros and cons of treatment variations
Lacrimal gland prolapse is still a topic of controversy among leading ophthalmologists who defend their point of view on the treatment of the disease. In its own way, each side is right, and at the same time, wrong. So there are two versions of treatment:
- complete removal of the third eyelid;
- reduction followed by suturing and return of the gland to its normal anatomical position.
Those who defend the first option motivate their point of view by the simplicity of execution, the expenditure of minimal time and money. Removal does not require a specially equipped ophthalmological office, equipment, or specific consumables. The procedure can be performed on a regular table using general sedation and the presence of the surgeon's hands and cutting instrument. The second advantage is the minimum rehabilitation time; after 2-3 days the animal is completely restored, no special eye care is required. And to rule out relapse, the lacrimal gland will no longer fall out.
Proponents of surgery appeal with the following arguments:
- the gland can be returned to its anatomically correct position;
- its function is preserved (production of tear fluid);
- the third eyelid remains mobile.
The most important thing is that the development of keratoconjunctivitis sicca is excluded; not all veterinarians remember this long-term complication, fixating on the immediate effect. This is a fundamentally wrong position, since a specialist must not only cure the existing problem, but also think about the future health of the animals.
Psychological aspects
Very often, the owners of dogs themselves, especially problem ones (Great Danes, Mastinos, Mastiffs, Newfoundlands), who almost always experience prolapse of the third eyelid due to breed predisposition, form the wrong attitude towards surgery. The roots of this are based on the fact that even after successful suturing, over time, the lacrimal gland again leaves its anatomical structures. There is a strong opinion among breeders that the operation does not help.
Another thing is that doctors who simply cut off the problematic gland enjoy fame among the owners, since I eliminate the problem for good. But few people think that in the future such dogs will have practically incurable eye problems that will be worse than prolapse.
Treatment Options for Lacrimal Gland Prolapse
The most popular are two types of techniques: “pocketing” and fixation of the lacrimal gland using various auxiliary devices. The most popular is the “pocket” and its modifications; it is simple, understandable and does not require complex specific equipment. The rehabilitation period after this technique is 5-7 days; the pet requires primitive care. Complications are rare; a lacrimal gland cyst develops (accumulation of tears in the cavity under the conjunctiva). But it can be prevented by leaving holes in the conjunctival recess. But this does not always work, since over time the drainage channels become overgrown.
The second, new “anchor” technique (purse-string suture), described in foreign sources in 2008, consists of forming a pseudopocket, but not through two incisions, but with the help of monofilaments that pass under the conjunctiva, “encircling” the gland. Significant advantages are that it is low-traumatic, painless, requires a minimum set of simple tools (tweezers, a clamp, non-absorbable monofilament) and speed of execution (5-7 minutes). The animal does not require specific care, the third eyelid is immediately tucked into place and its mobility is maintained, daily care - eye drops for 3-5 days (chloramphenicol).
At the Ros-Vet VC, ophthalmological operations of any complexity are performed. If your pet has visually noticed third eyelid prolapse, don’t hesitate! It is important to perform surgery on time. Call and come to the Ros-Vet Exhibition Center.
Hyperplasia or prolapse of the lacrimal gland of the third eyelid
The third eyelid (or nictitating membrane) serves to provide additional protection to the eyeball in animals. The shape of the third eyelid is given by a very thin T-shaped cartilage, which, due to its rigidity and elasticity, supports its internal frame. In the thickness of the third eyelid, the T-shaped cartilage is surrounded by a gland that takes an active part in moisturizing the eyeball - this is an additional lacrimal gland, producing approximately 30% of the tear fluid. As the third eyelid moves, tears are distributed over the surface of the cornea, simultaneously washing away foreign particles and bacteria from it. The inner surface of the third eyelid is lined with bright pink tuberous lymphoid tissue, consisting of many follicles - this is the most powerful unit of the immunological protection of the eye.
In dogs, the third eyelid is usually pigmented with brown-black pigment, but it can also be devoid of pigment, a pale pink color - this is especially noticeable by the color of the edge of the third eyelid (about 2 mm) in the inner corner of the eye. The absence of pigment is not a pathology. However, it is believed that the non-pigmented mucous membrane of the third eyelid and conjunctiva is more sensitive to the damaging effects of ultraviolet rays and irritating environmental factors.
Under certain conditions, the gland of the third eyelid can increase in volume and fall out, i.e. appear between the cornea and the third eyelid in the form of a ridge or rounded swelling.
Lacrimal gland prolapse (other names: third eyelid adenoma, “cherry eye”) usually occurs in young dogs under 1 year of age, during a period of active growth, usually around 3-6 months. Most often, dogs of brachiocephalic breeds (bulldogs, pugs), dogs with a loose constitution and a large head (cane corso, mastiffs, Newfoundlands, Great Danes), with a pronounced transition from the forehead to the muzzle (American cocker spaniels, Cavalier King Charles spaniels, Shar Pei, Chow Chow), but the disease is also often found in Beagles, Basset Hounds, and Bloodhounds.
Etiology
The causes of prolapse of the lacrimal gland of the third eyelid are: · weakness of the ligaments that hold it in its normal position, · eversion of the base of the cartilage of the third eyelid, · neoplasms of the lacrimal gland (adenoma), · hyperplasia of the third eyelid gland due to leukemia, · genetic predisposition, · factor initiating rupture The ligament that holds the gland in place may be an injury to the third eyelid (self-injury during play, scratching with paws).
Symptoms
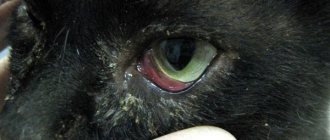
Prolapse of an enlarged third eyelid gland between the edge of the third eyelid and the cornea is quite common in young dogs. It is observed in the form of a round, intensely pink swelling with a diameter of up to 10-15 mm that periodically or constantly appears in the inner corner of the eye (the so-called “cherry eye”). The conjunctiva is inflamed, follicular hypertrophy, lacrimation, and purulent mucous discharge may occur over a long period of time. Initially, the disease is one-sided, but often after 1-3 months the second eye is also involved in the process.
Treatment
Inflammation, even in the presence of infection, is not the root cause of the disease, so the use of corticosteroids and antibiotics is ineffective.
Repositioning the gland does not bring results, since in the absence of fixation in the normal position, the gland will fall out again within a few days, sometimes within a few minutes after the manipulation.
Treatment of this pathology is only surgical and should be aimed at repositioning and fixing the prolapsed lacrimal gland in a normal position to the periosteum of the zygomatic bone. The operation is performed under general anesthesia. If during surgery it is possible to establish weakness of the ligamentous apparatus of the gland of a healthy eye, its simultaneous preventive fixation is indicated.
There are various options for this operation, but the criteria for the correct technique are as follows: 1. The prolapsed glandular tissue must be completely preserved. 2. The integrity of the third age must not be compromised. 3. Upon completion of the postoperative period, the mobility of the third eyelid (its functional characteristics) should be completely restored.
Removal of the gland or cartilage of the third eyelid is carried out only as a last resort (in the presence of neoplasms), because after removal of the gland responsible for a significant part of the production of tear fluid, there is a high probability of developing dry eye syndrome, pigmentary keratitis and, as a result, pain and loss of vision. Lack of necessary skills and experience cannot justify resection of prolapsed glandular tissue or the third eyelid. Given the predisposition of beagles to the disease keratoconjunctivitis sicca, removing the third eyelid in a dog of this breed would be a serious medical error.
In the postoperative period, the use of anti-inflammatory drops containing broad-spectrum antibiotics is indicated for 7-10 days. Wearing a protective collar is mandatory. The efficiency of the operation is 60%-90%.
LOSS (PROLAPS) OF THE THIRD EYELID
Prolapse of the third eyelid should be distinguished from prolapse of the third eyelid gland.
Complaints from dog and cat owners that “the third eyelid suddenly popped out and covered half the eye” are encountered quite often in veterinary practice and sometimes baffle general practitioners. This phenomenon is most often not an eye pathology, but a syndrome of certain diseases.
With unilateral prolapse of the third eyelid, it is necessary to exclude: - Foreign body behind the third eyelid, damage to the cornea, trauma (bite, puncture of the third eyelid), inversion of the third eyelid, entropion of the eyelids. - Atrophy of the eyeball. — Inflammatory process/neoplasm of the maxillary, nasal bones, orbit. — Retro- and parabulbar abscesses and hematomas. — Syndrome of impaired sympathetic innervation (Bernard-Horner syndrome). — Paresis/paralysis of the facial nerve.
With bilateral prolapse of the third eyelid, it is necessary to exclude: - Foreign body behind the third eyelid, damage to the cornea, trauma (bite, puncture of the third eyelid), inversion of the third eyelid, inversion of the eyelids. — Lesions of the central nervous system (hemorrhages, neoplasms in the midbrain, medulla oblongata and brain stem); syndrome of impaired sympathetic innervation (Bernard-Horner syndrome). — Severe intoxication, dehydration, cachexia. — Helminthic infestations, latent viral infections (without pronounced clinical signs), stress.
As is clear from the above, there is no treatment for third eyelid prolapse as such. When the underlying cause of the disease is eliminated, the third eyelid gradually restores its normal position.
Conclusions from the above:
- In general, the phenomenon of prolapse or prolapse of the lacrimal gland of the third eyelid has become more common. This is due both to the trend in breeding short-faced rabbits and to the lack of targeted work on the formation of a breeding herd, taking into account the predisposition of rabbits to this defect.
- When you next examine your rabbits, be sure to check the condition of their eyes. Pay attention to the slightest redness of the eyeballs and eyelids, the absence of foreign objects. Check to see if there is excessive tearing? If the slightest increase in the third eyelid begins, contact a veterinarian.
- Do not leave for offspring rabbits that have experienced the phenomenon of prolapse, or if there have been such cases in their family. After all, it is impossible to reliably determine whether the cause of the pathology is injury or a congenital defect.
- Share information with your friends and colleagues. Only the massive adoption of measures to eradicate the innate tendency of rabbits to prolapse can stop the negative trend in the industry as a whole.