Intervertebral disc diseases are a common pathology in veterinary practice, which can lead to serious neurological disorders with irreparable consequences and require immediate contact with a veterinary center for help.
“Intervertebral disc disease” is an umbrella name for a number of spinal diseases in dogs. In this article we will look at typical intervertebral disc diseases, such as Hansen type 1 intervertebral disc disease, Hansen type 2 and separately intervertebral disc disease, which leads to the development of lumbosacral stenosis.
Intervertebral disc disease manifests itself with various clinical signs depending on the affected part of the spine, and the degree of neurological deficit ranges from minimal pain to paresis or paralysis.
With this disease, using a neurological examination, the doctor evaluates the reflex reaction of the thoracic and pelvic limbs, postural reactions and the presence of deep pain sensitivity. Based on these criteria, the degree of neurological deficit is judged and a possible prognosis for the animal’s recovery is given.
In the initial stage of the disease, such patients may end up in a veterinary clinic with seemingly different symptoms. A frequent complaint of dog owners during this period of disc disease is pain of unknown etiology, and sometimes owners confuse this problem with abdominal pain and other disturbances in the normal condition of the pet. In this regard, it is extremely important to thoroughly understand the cause of pain in a dog, conduct a truly informative and necessary diagnosis to make the correct diagnosis and prescribe the necessary treatment.
Etiology
The cause of intervertebral disc disease is destructive changes in the disc itself as a result of cartilaginous metaplasia. There are also predisposing factors such as genetic predisposition (chondrodystrophic dog breeds), obesity, age from 3 to 6 years and, very rarely, spinal injury.
To better understand the occurrence of this process, you need to have a good understanding of the pathological physiology of the disease, which we will try to explain in a brief summary.
When the dog moves, the intervertebral disc serves as a load distribution in the spine, ensuring its stability and supportability. The intervertebral disc (IVD) itself is quite simple from an anatomical point of view. On the outside, it is represented by a fibrous ring consisting of collagen fibers that connect to the cartilage of the endplates of the vertebral bodies.
The external collagen fibers are connected to the ventral (lower) and dorsal (upper) longitudinal ligaments. In turn, the collagen fibers of the fibrous ring are connected to the internal structure of the intervertebral disc - the nucleus pulposus, which contains a large number of water molecules. In addition to water, the molecular composition of the intervertebral disc contains collagen and non-collagen proteins, a complex of proteoglycans and glycoproteins. Glycosaminoglycans (GAGs) are represented by proteoglycans. Their highest concentration is observed in the core of the intervertebral disc, where they are needed to bind water molecules.
Thus, with progressive pathological processes associated with disease or age, the concentration of proteogicans sharply decreases, which leads to a decrease in the concentration of water molecules in the nucleus pulposus and the fibrous ring of the intervertebral disc.
As for the age-related aspect of the disease, the aging process of the intervertebral disc is represented by fibroid metaplasia. The reason for this process is also associated with a decrease in the number of proteoglycans and, accordingly, water molecules in the disk. Chondrodystrophic breeds of dogs are predisposed to fibroid metaplasia, that is, to premature aging of the intervertebral disc.
.
Intervertebral disc diseases are divided into 2 types.
Hansen type 1 intervertebral disc disease is an extrusion (herniation) of the disc contents, that is, the nucleus pulposus, into the lumen of the spinal canal, which leads to compression of the spinal cord. The process of loss of disc contents occurs quite quickly or even at lightning speed, which characterizes the acute course of the disease and the development of corresponding clinical signs. Middle-aged dogs between 2 and 6 years old are predisposed to this type of intervertebral disc disease, and most often these are chondrodystrophic dog breeds, such as dachshunds, bulldogs, and pugs. In these dog breeds, degenerative disc changes can begin at an early age, around 3 months. Therefore, dogs with a herniated intervertebral disc that are not included in the above age category are often brought in, for example, at one year of age.
In 65-71% of cases, herniated discs are formed at the level of Th 11 and L2. (Brown NO, Helphrey M.L., 1977, Hoerlein BF Oliver JE, 1987). The next place in terms of frequency of damage (6-7%) is occupied by the cranial part of the cervical spine (C2-NW and C3-C4). In third place are the lumbar vertebrae (L2-L3 and L3-L4) (Hoerlein BF, 1987). There is an almost complete absence of herniated intervertebral discs at the Th 1-Th 10 level, which is explained by the presence of the rib cage and the ligament that fixes the heads of the namesake ribs.
Hansen type 2 intervertebral disc disease is characterized by gradual bulging of the annulus fibrosus into the lumen of the spinal canal without rupture, which leads to gradual compression of the spinal cord.
This type of disease is characterized by a slowly progressive course and occurs in older dogs from 6-7 years of age. Degenerative changes in the disc with this type of disease occur gradually. Non-chondrodystrophic dog breeds, such as German and East European Shepherds, Labradors, and Golden Retrievers, are predisposed to this type.
Hansen type 2 intervertebral disc disease also includes degenerative lumbosacral stenosis (cauda equina syndrome) or lumbosacral stenosis. With this pathology, between the last lumbar vertebra and the sacrum (segment L7-S1), the intervertebral disc undergoes degenerative changes and it bulges into the lumen of the spinal canal with compression of the nerves in this segment - compression of the cauda equina. This type of intervertebral disc disease belongs to Hansen type 2 with the formation of osteophytes in the area of the foramen and osteophytes in the area of the vertebral endplates. Middle-aged and elderly dogs of the following breeds are predisposed to lumbosocral stenosis: German Shepherd, Labrador Retriever, Border Collie.
Consequences of non-treatment
If the owner treats his pet irresponsibly, an abscess can result in various complications and consequences for the dog. Failure to treat external problems leads to infection of the subcutaneous areas and abscess of the animal’s internal organs. Often, due to lack of attention to the disease, sepsis develops - systematic blood poisoning with infections.
Deep abscesses open inside the body, and pus leaks into the dog. Pus entering the abdominal cavity can lead to peritonitis.
Failure to treat any form of abscess will most likely result in the dog's premature death.
Ulcers in dogs can occur in the form of pyoderma, abscesses, dermatitis, abscesses of varying etiology and severity. Not always pustules can lead to serious consequences, but in some cases the lesion can affect the deep layers of the skin and subcutaneous tissue, leading to purulent melting of the tissue. To prevent serious complications, you need to know the signs and methods of treatment.
Clinical signs
Clinical signs of intervertebral disc disease depend on the location of the problem, the type of disease and the degree of spinal cord compression.
With Hansen type 1 intervertebral disc disease, the animal may experience pain and neurological disorders in the form of weakening and absence of motor function of the limbs, decreased or absent deep pain sensitivity, and impaired urinary function. Such animals often experience hyperesthesia - pain in the region of the segment of the spine where the hernia occurred. Pain develops due to compression of the nerve roots or membranes of the spinal cord. If the hernia has prolapsed unevenly, that is, into the right or left side of the spinal canal, then the neurological deficit may be more pronounced on the side of the hernia prolapse.
Hansen type 1 intervertebral disc disease is characterized by an acute course, most often with the development of severe pain and neurological deficit. In the initial stages of the disease, clinical signs at first glance may be atypical for this pathology and resemble pain in the abdominal cavity due to the manifestation of hyperesthesia. Further, with the development of compression, neurological disorders will be observed depending on the location of the problem.
In Hansen type 2 intervertebral disc disease, the clinical signs will be similar to Hansen type 1, but the course of the disease will develop slowly, they also depend on the location of the problem.
Compression damage to the spinal cord due to intervertebral disc disease is characterized by:
With intervertebral disc disease Hansen type 1 or type 2 in the cervical spine in the segment from 1 to 5 cervical vertebrae in animals, the following clinical signs are observed: pain syndrome, proprioceptive ataxia; with central compression, impaired motor function of all limbs can develop - tetraparesis, and with compression on one side – hemiparesis. During a neurological examination, all reflexes in the limbs will be enhanced. Spasticity and hypertonicity of all extremities may also be observed.
These clinical signs are characteristic of all types of intervertebral disc disease, the difference will be in the development of clinical signs: with Hansen type 1, clinical signs will develop quickly and the degree of neurological deficit can go from 1 to 5 in a few minutes. In Hansen type 2, the course of the disease is always chronic, and the neurological deficit gradually progresses.
Typically, at the reception, such animals can only show pain when turning the neck, lifting the dog in your arms, or any other movement - this is the initial stage of the disease. In this case, they speak of the first degree of neurological deficit.
In the future, the dog may develop more serious cynic signs. There may be loss of the ability to move, which is expressed in proprioceptive ataxia of all extremities with the presence of deep pain sensitivity. If the hernia or protrusion is located in the right or left half of the spinal canal, then the neurological deficit of the limbs may be observed more on the side of the prolapse of the hernia or protrusion. In this segment of the spine, it is extremely rare that a compression problem can lead to tetraplegia with loss of deep pain sensitivity, since the spinal canal here is quite wide. In this case, the reflexes of the limbs are enhanced.
With disc disease in the C6-T2 segment (from the sixth cervical to the second thoracic vertebrae), the clinical signs will be similar, but there are also specific features. A similar characteristic clinical sign is pain when moving the neck, namely when lifting the dog. The peculiarity lies in the results of the neurological examination: there is proprioceptive ataxia, a decrease in the sensitivity of the thoracic limbs, and unevenly. That is, sensitivity and decreased reflexes will be more pronounced on the side of the hernia prolapse. During a neurological examination, the reflexes of the thoracic limbs will be reduced, since the nerve roots that form the brachial plexus originate in this segment of the spinal cord, and the reflexes of the pelvic limbs will be strengthened.
Problems with the innervation of the bladder in compression pathologies of the cervical spine are extremely rare or only in particularly advanced cases.
In case of intervertebral disc disease in the T3-L3 segment (from the third thoracic to the third lumbar vertebra), the thoracic limbs will be intact, that is, without changes. In the initial stage, such animals may develop pain in the back, pain when moving, and a hunched gait. In more severe stages, proprioceptive ataxia of the pelvic limbs occurs, their motor function is impaired, urination disorders, atony, and a decrease or absence of deep pain sensitivity are noted. Reflexes of the pelvic limbs are strengthened or normal.
With disease of the intervertebral discs in the L4-S3 segment - the “cauda equina” (from the fourth lumbar vertebra to the sacrum), signs of damage to the peripheral neuron are observed, that is, the thoracic limbs will be intact, and reflexes on the pelvic limbs will be reduced or absent altogether. Pain, proprioceptive ataxia, and paresis or paralysis with decreased or absent deep pain sensitivity may occur. Compression damage in this segment of the spinal cord leads to dysfunction of the lumbosacral thickening, respectively, to neurological deficits of the femoral, sciatic, pudendal and pelvic nerves. In such animals, muscle atrophy quickly develops, and the tone of the anal sphincter and bladder is reduced or absent. Atony of the bladder may develop, and urination and defecation are disrupted.
Damage to the caudal segments of the cauda equina is characterized by dysfunction of the sciatic, pudendal, pelvic and caudal nerves. Since the femoral nerve is not affected, the animals retain the ability to walk, but the hock joints will be lowered. The knee reflex is normal.
In case of intervertebral disc disease, it is customary to use the following gradation when determining the degree of neurological deficit:
1st degree – the animal experiences only pain syndrome without neurological deficit;
2nd degree – pain syndrome and mild degree of neurological deficit – ataxia (gait disturbance);
3rd degree – tetraparesis or paraparesis, urination disturbance;
4th degree – tetraplegia or paraplegia in the presence of deep pain sensitivity;
5th degree – there is no deep pain sensitivity;
Grade 6 – deep pain sensitivity is absent for more than 48 hours.
Discopathy in dogs, discopathy in dachshunds and other breeds.
What is discopathy? This is a change in the structure of the intervertebral disc. Imagine that it was elastic, capable of acting as a shock absorber. But its structure has changed, it has lost its elasticity.
This is called degenerative changes. And such a disc can migrate from its usual location between the vertebrae. It enters the spinal canal. This is a tube consisting of bone tissue, and inside it is the spinal cord (like a train in a subway tunnel). The disc fills the space between the spinal cord and the spinal canal and begins to compress the spinal cord, disrupting its blood circulation, which leads to the death of nerve cells and loss of motor function of the limbs. The stronger the pressure of the disc on the brain, the more blood circulation suffers, the worse the prognosis. The motor function always falls out first, and then the sensitive one. When the last forecast is bad!!!
Our clinics provide diagnostics and surgical treatment of discopathy, prices are 30-50% lower than in Moscow clinics. Sergey Aleksandrovich Yagnikov operates . You can make an appointment by calling 8-915-285-37-21.
Rice. 1. Spinal cord due to compression by disc herniation. Bulging of the swollen spinal cord after opening the membranes (1) . Segment of swollen spinal cord with preserved membranes (2.) . Myelomalacia (melting, liquefaction) of the spinal cord due to the death of nervous tissue (3) . The spinal cord “leaks out” (3) .
Can the owner of the animal influence these changes through feeding or nutritional supplements or medications - no!
What does a pet owner need to know about discopathy? The first is that breeds such as dachshunds, cocker spaniels, and French bulldogs have a predisposition to this pathology. The second thing is that this is an urgent pathology, i.e. if the owner of the animal does not go to the clinic in time, and the clinic’s doctors are unable to urgently provide qualified assistance, then the animal may permanently lose the ability to move (usually the pelvic limbs), control over urination and defecation.
But how can a pet owner understand that his pet has discopathy? Well, first of all , remember about the breed predisposition (dachshunds, etc.). The second is typical symptoms: rapid development of the disease, the animal hunches its back, the pelvic limbs are “tangled”, the animal cannot jump onto the sofa, the stomach is tense, “stilted gait”, the animal groans. Moreover, not all symptoms can appear simultaneously. If the animal completely “drags” the pelvic limbs, then if it matches the breed, this is almost 100% discopathy.
What is the treatment strategy for a herniated disc? It depends on the clinical symptoms at the time of visiting a doctor. If the animal walks, hunches its back, and its pelvic limbs are slightly tangled, then with such symptoms the animal is limited in movement for 14 days, and corticosteroid hormones are prescribed (metipred 10 mg/kg body weight intravenously) against the background of drip infusions, or a single injection subcutaneous dexafort (prescribed only after consultation with a doctor). If the animal does not get worse, this means that the disc is no longer displaced. Within 14 days, the hole through which the disc moved into the spinal canal and compressed the spinal cord will heal and the remaining mass of the disc will no longer “cause a problem.” But if the animal is worse, it is necessary to undergo surgery!
If the animal walks poorly, and practically drags its pelvic limbs or does not walk at all (but the hind legs feel pain), then it is necessary to urgently undergo surgery!!!
If the animal completely drags its pelvic limbs and they do not feel pain, the prognosis is unfavorable (the animal will most likely never walk).
Why is it so important to correctly determine in an animal dragging its pelvic limbs whether they feel pain or not? The prognosis for the restoration of motor function depends on this. If the pelvic limbs feel pain, then the animal will eventually walk, but if not, then it will never walk! But what is the manifestation of pain? This is an animal's reaction to irritation. If you squeeze the skin between your fingers tightly (with a needle holder), the animal will whine, turn its head, and try to bite you, but the feeling of pain is preserved. And if he just pulls or twitches his paw, then this is just a reflex and the prognosis is bad!
The first animal with paralysis of the limbs has no pain sensitivity, while the second animal with paralysis of the limbs has it preserved. And the second animal will walk!
Many people say “...we were offered surgery, but the chiropractor set my dachshund’s disc and my animal began to walk”! The disc is a mass similar to cottage cheese, and it cannot be straightened! And your animal went because pain sensitivity was preserved, and this is a sign that the spinal cord was damaged “not very much”! My colleagues and I propose surgery because surgery gives a much greater chance of recovery, and the technology for surgical intervention and caring for an animal is almost 100% perfect today. But if you don’t do the operation and the disc continues to shift at some point, then the prognosis will be bad!!!!
What is the essence of the operation? Remove a herniated disc - remove pressure on the spinal cord, reduce swelling, improve blood circulation in the spinal cord by opening its membranes. If necessary, perform vertebral stabilization. But before undergoing surgery, it is necessary to determine exactly at what level the intervertebral disc has fallen out. To do this, it is necessary to perform myelography (contrast spondylography), i.e., inject a contrast agent under the membranes of the spinal cord to see its contours on an x-ray.
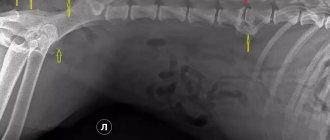
Norm. Two columns of contrast agent (white lines) “above and below” from the spinal cord, smooth without bends.
Disc herniation at the level of 11-12 thoracic vertebrae ( ). Arc-shaped displacement of the lower contrasting column.
Operation stages:
Removal of the vertebral wall (hemilaminectomy) (1) to visualize the spinal cord (2) . Removal of a herniated disc (3) . Opening the dura mater (4) .
Diagnostics
Problems in diagnosing intervertebral disc disease can arise in the early stages with 1 degree of neurological deficit. At the onset of the disease, clinical signs may be atypical and often manifest only as pain. When a neurological deficit occurs, there are usually no problems with diagnosis.
Intervertebral disc disease can be diagnosed through a neurological examination of the animal and special studies.
During the examination, we determine the degree of neurological deficit, the approximate localization of compression of the spinal cord or nerve roots, which is important for further research. The prognosis for the animal’s recovery depends on the degree of neurological deficit.
Special tests to detect the disease include radiographic examination, myelography, computed tomography (CT) and magnetic resonance imaging (MRI), and in some cases myelo-CT.
X-ray examination can be informative in identifying this problem, but it does not provide accurate localization of the prolapsed contents of the hernia.
X-ray signs of Hansen type 1 disc disease include narrowing of the intervertebral space, the intervertebral foramina, and the space between the articular processes. If the core of a prolapsed disc has become calcified, it can sometimes be seen in the spinal canal, but this is extremely rare. With Hansen type 2 intervertebral disc disease, a different picture can be seen on x-rays. For chronic problems, typical signs, in addition to narrowing of the intervertebral space and foramina, are sclerosis of the articular plates of the vertebrae, the formation of osteophytes, spondylosis, etc. This is especially pronounced in lumbosacral stenosis (“cauda equina syndrome”).
X-rays are not reliable for identifying the source of compression. In this case, myelography, MRI or CT is used.
Myelography is a standard method in diagnosing intervertebral disc herniations. As a result of the study, weakening or absence of contrast may be noticed in places of spinal cord compression. This diagnostic method has its drawbacks - it is invasive and not very good visualization of the affected area in the presence of hemorrhage and swelling of the spinal cord.
The most informative method for diagnosing intervertebral disc diseases is MRI or CT. These studies are more accurate and non-invasive.
On a CT scan, intervertebral disc extrusions will appear as a bright spot (weakened signal). In different planes on CT, herniated discs can be clearly interpreted in sagittal, axial and coronal sections. It is possible to clearly determine its length and location, which provides more information for treatment than a conventional x-ray. In some cases, when a herniated disc has the appearance of an extradural formation with strong signal attenuation, for example, the contents of the disc with blood, it makes sense to perform a myelo-CT.
MRI diagnostics for intervertebral disc disease allows you to better see the injury or any other consequences of a prolapsed hernia or long-term compression of the spinal cord. Using MRI diagnostics, it is possible to recognize early degeneration of the intervertebral disc: in T2 mode, the disc will have a decrease in signal intensity - the disc will be dark. The prolapsed contents of the disc in the T2 mode in the lumen of the spinal canal will also be dark, and subsequent prolapse of the hernia - edema, necrosis or inflammation will have a hyperintense signal. Using MRI diagnostics, you can assess the prognosis for recovery: if the hyperintense signal from the spinal cord is equal to or greater than the length of the L2 body (second lumbar vertebra), then the prognosis for recovery is 55%, and with loss of deep pain sensitivity only 10%.
Treatment of the disease
Therapy at home is possible with the help of medications or folk remedies. Self-treatment at home lasts no more than 10 days; if the disease progresses during this period, you should urgently contact a veterinarian. But in 90% of cases everything is treated without complications.
Therapy with pharmaceutical drugs
First you need to disinfect the skin; for this, antiseptics are used to treat wounds (hydrogen peroxide, furatsilin, potassium permanganate, iodine or brilliant green). Among them, peroxide is considered the most painless for dogs. The procedure should be carried out 3-4 times a day.
Secondly, if there are ulcers, you need to apply bandages using traction agents. The faster the drug eliminates pus from the wounds, the faster the dog will recover. The most popular pulling agents:
- Vishnevsky ointment;
- Levomekol;
- Ichthyol ointment;
- Tetracycline ointment;
- Syntomycin liniment.
Taking antibiotics requires consultation with a veterinarian, but their use is highly recommended. It is not necessary to take your dog to the clinic; you can consult about medication over the phone. If there is severe pain, painkillers are also prescribed (Analgin can be given).
To strengthen the dog's immune system and overall well-being during treatment of an abscess, vitamin complexes such as Hokamix30, AniVital CaniAge or Excel 8 in 1 can be used.
Herbal treatment
The use of folk remedies pursues the same goals as drug treatment: disinfection, drawing pus from wounds, pain relief and general strengthening of the body. First of all, it is recommended to apply compresses to wounds using celandine:
Dilute canned and freshly squeezed celandine juice with vodka 1 to 4. Soak gauze in the solution and apply to the site of the abscess. The dog should wear the compress 2-3 times a day for 10 minutes.
The recipe for St. John's wort and calendula heals wounds well. To prepare, you need to boil a glass of water, add 20 drops of a mixture of juice of two herbs to the cooled water. Add a pinch of salt. Soak gauze in the solution and apply to the wound 2-3 times a day. The effect of use should be noticeable before the end of the first day of such treatment.
Echinacea or ginseng root are used to strengthen the immune system. Decoctions of nettle, chamomile, plantain and millennial also have antiseptic properties.
Opening an abscess in a dog
Opening an abscess should be performed by a specially trained veterinarian. We do not recommend trying to perform essentially a surgical operation on an animal yourself. With severe progression of the disease, neglect or accumulation of a large amount of pus, veterinarians resort to deliberate opening of the abscess. The sequence of performing the operation in the clinic:
- Antiseptic treatment and pain relief with lidocaine or another drug;
- An incision with a scalpel in the area of the purulent head;
- Expansion of the incision using a Hartmann syringe;
- Suction of pus and cleansing of the resulting cavity;
- Washing with antiseptic agents.
Removing abscesses in dogs lasts from 5 to 30 minutes and is practically painless for the pet. In some cases, drainage and a special tube are installed to drain pus in the future if the doctor believes that treatment may be delayed.
There are cases when a dog's abscess opens on its own. The owner must treat the wound, bandage the area and take the sick dog to the doctor.
Treatment
Treatment of intervertebral disc disease can be therapeutic or surgical. The choice of treatment primarily depends on the neurological condition of the patient and the frequency of relapses of the disease.
Therapeutic treatment is used for the first degree of neurological deficit or progressing to the second. Such treatment consists of restricting mobility and using painkillers and anti-inflammatory drugs. From the group of non-steroidal anti-inflammatory drugs, a fairly extensive list is used, but in our clinic they most often use Loxicom or Previcox.
Of the corticosteroid drugs, it is recommended to use Methylprednisolone or Prednisolone. During therapeutic treatment, it is necessary to understand the risk of deterioration of the animal's neurological condition, especially if the movement restriction regime is not followed.
It is important to know that it is impossible to return the intervertebral disc substance to its anatomical position with any medications.
Most often, only surgical treatment provides a complete recovery. With conservative treatment, we try not to provoke further prolapse of the altered nucleus pulposus and relieve swelling of the spinal cord.
Surgical treatment involves decompression and removal of part of the disc or prolapsed disc contents.
The type of surgical treatment depends on the part of the spine and the type of intervertebral disc disease itself.
For Hansen type 1 intervertebral disc disease, starting from degree 2 of neurological deficit, the following are used:
- hemilaminectomy;
- minihemilaminectomy;
- ventral slot.
Hemilaminectomy
and
minihemilaminectomy
are used for herniated discs in the thoracic and lumbar regions.
Progress of the operation:
A skin incision is made at a distance of 2-3 cm from the spinous processes. The superficial fascia is divided bluntly and access to the lumbodorsal fascia is opened, then it is dissected at a distance of 1 cm to the side of the spinous processes.
At this point, the muscles are separated from the spinous and articular processes using a blunt method, without touching the spinal nerve and blood vessel emerging from the intervertebral foramen. The cranial mastoid and articular processes are removed. A bone gap is formed at the site of the removed processes.
Both techniques are similar in terms of surgical approach, but there is a fundamental difference between them. Minihemilaminectomy is less traumatic, that is, the iatrogenic impact on the spinal cord is minimal.
Ventral cut
used for herniated intervertebral disc in the cervical spine.
Progress of the operation:
A linear skin incision from the larynx to the sternum. The muscles are divided using the blunt method (sternocephalic, sternohyoid). The trachea and esophagus are shifted to the left side. Next, between the paired long muscles of the head, access is made to the paired long muscle of the neck, the fibers of which are obliquely attached to the cervical vertebrae. The bone gap is formed using a bone cutter. The length of the gap on each side is from 1/4 to 1/3 of the length of the vertebral body, the width, depending on the size of the dog, is from 3 to 5 mm, but not more than half the width of the vertebral body. Next, the surgical wound is sutured.
For the syndrome of lumbosacral stenosis of the cauda equina
decompression of L7-S1 is carried out, the contents of the prolapsed disc and part of the fibrous ring are removed.
Next, the segment is stabilized using wires with inert cement. Now, for stabilization, transpedicular fixators have begun to be used, which have proven themselves to be a very reliable type of fixation with the least surgical complications. This technique is used in our clinic.
Treatment of intervertebral disc disease in dogs
Treatment can be therapeutic, but it will be effective only when, of the entire symptom complex, only pain is observed. In this case, treatment includes restriction of mobility, prescription of non-steroidal anti-inflammatory drugs and corticosteroids.
For this pathology, the most effective surgical treatment is decompression of the hernia site (cutting out a section of the vertebra and removing the herniated disc).
Methods of surgical treatment
- Hemilaminectomy and minihemilaminectomy are used for herniated discs in the thoracolumbar spine.
Hemilaminectomy. - Ventral cut (ventral slot) is used for herniated intervertebral disc in the cervical region.
Ventral cut (ventral slot).
The prognosis after surgery depends on many factors: the degree of neurological deficit, the duration of the disease, the patient’s health status, the location of the lesion, and so on.
Forecast
The prognosis for intervertebral disc disease depends on many factors: time, degree of neurological deficit, and so on.
Comparative prognosis for cure:
| Neurological picture | Type of treatment | Prognosis for therapeutic treatment | Prognosis for surgical treatment |
| Paraplegia, absence of HBC | 24-48 hours – surgical decompression. More than 48 hours – surgery is not recommended | 5% | 24-48 hours - 45-76%. More than 48 hours – 6-33% |
| Paraplegia, there is GBH. No superficial sensitivity | Surgical decompression | 50% | 86-89% |
| Paraplegia, HBH yes | Surgical decompression | 51% | 79-96% |
| Paraparesis, lack of mobility | Surgical decompression | 55-85% | 83-95% |
| Paraparesis, ambulation function present | Therapeutic treatment | 55-85% | 83-95% |
| Only pain syndrome | Therapeutic treatment | 55-85% | 83-95% |
Clinical case of treatment of BMPD in a dachshund
A dachshund named Nice was admitted to the Pride Center on June 13, 2017 because a week ago she became more constrained, and the day before her appointment she stopped walking. At an appointment with an orthopedic neurologist, a neurological examination was carried out, as a result of which a neurological deficit of both pelvic limbs of the 2nd degree, progressing to the third, was discovered, and a preliminary diagnosis was made - intervertebral disc disease in the thoracolumbar spine. After a mandatory examination before anesthesia, Nice was sent for a CT scan.
A CT scan confirmed a hernia of the intervertebral disc Th13-L1 on the left with extrusion of the nucleus and visible overlap of the spinal canal up to 60-80%. With such a degree of spinal canal obstruction, it is very important to undergo surgical treatment as quickly as possible in order to get the best result. And on the same day, the neurosurgeon performed a hemilaminetomy operation, which consists of decompression and removal of the prolapsed contents of the disc.
After the operation, Nice remained under the supervision of doctors in the hospital, and the next day she went home. Nice is now undergoing rehabilitation and recovering.
Veterinary surgeon, specialist in traumatology, orthopedics and neurology Maslova E.S. Veterinary anesthesiologist Orlovskaya M.V.
Author of the article: veterinary surgeon, specialist in orthopedics, neurology and neurosurgery Ekaterina Sergeevna Maslova
Abscess in dogs
Our four-legged friends lead a very active lifestyle; often fun games in the fresh air end in microtraumas, in the place of which an attentive owner can discover huge bumps in a few days.
The sight of huge abscesses often frightens dog owners, but there is no need to worry. Timely contact with a specialist and competent treatment will save your beloved pet from abscesses without consequences; independent treatment of abscesses or advanced stages of the disease can lead to the development of sepsis and the death of the animal.
An abscess in dogs is a focal purulent inflammation of tissue. The causative agent of the disease is a pathogenic microflora, most often Staphylococcus aureus or white, penetrating from the outside through damaged skin or hematogenously from a pathological focus. Depending on the location, external and internal abscesses are distinguished. Internal abscesses form in internal organs and tissues during infectious and non-infectious diseases; external abscesses occur most often from bites, scratches, wounds, inflammation of the anal glands, and deterioration of the immune system.
Characteristic is the formation of a cavity separated from healthy tissue by a demarcation line. At the site of penetration of pathogenic microflora, an inflammatory process occurs, accompanied by swelling and the proliferation of staphylococci and streptococci. In response, the animal’s body produces lymphocytes, which form a kind of capsule that prevents the further spread of pathogenic microflora. As it matures, pus forms inside the abscess, consisting of dead blood cells, lymphocytes and pathogenic microbes.
Subcutaneous abscesses are easily detected by the dog's owner when the skin becomes red with the further formation of a soft swelling filled with pus, which, after the abscess has matured, comes out and the wound heals. The presence of internal abscesses can be assumed only by the lack of appetite, progressive emaciation and fever of the pet.